Is a new coronavirus variant behind California's Covid-19 rise?
Los Angeles, California - Coronavirus transmission is once again spiking in California entering the winter holiday season – and a new subvariant may be partly to blame, officials say.
This latest subvariant, JN.1, is now estimated to account for roughly 44% of Covid-19 cases nationally, according to the latest data from the US Centers for Disease Control and Prevention (CDC).
That share is twice as high as any other identified subvariant, and a startling rise from the prior estimate of 21% for the two-week period that ended December 9.
"We're also seeing an increasing share of infections caused by JN.1 in travelers, wastewater and most regions around the globe," the CDC said in a statement. "JN.1's continued growth suggests that the variant is either more transmissible or better at evading our immune systems than other circulating variants."
The World Health Organization this week classified JN.1 as a "variant of interest," meaning it has potentially concerning characteristics – such as an ability to more easily infect individuals or avoid the protection afforded by vaccines and therapeutics.
Current vaccines, anti-Covid drugs, and tests continue to work well against JN.1, the CDC said.
The rise of the JN.1 coronavirus variant

JN.1 is an offshoot of another omicron subvariant, BA.2.86, which was unofficially nicknamed Pirola.
Pirola was already deemed worrisome because of its unusually high number of mutations, which might empower it to more easily infect those who haven't received a recent Covid-19 vaccination. JN.1 has an additional mutation.
Experts say all those mutations mean it's likely that people who have been relying on older vaccinations received more than a year ago, or a previous infection earlier this year, may not be protected enough to avoid a new run-in with the coronavirus this winter.
"It is possible that at least part of the local increase in transmission is driven by new Covid-19 strains gaining dominance in Los Angeles County, including JN.1," the county Department of Public Health said in a statement.
Doctors say the rise of JN.1 is another reason why people – especially those who are older – should get the latest Covid-19 vaccination that became available in September.
Coronavirus transmission and Covid-19 hospitalizations, though undoubtedly on the rise, aren't at the levels seen at this same time last year.
But the increase has been sharp. For the week ending December 16, there were 2,924 new coronavirus-positive hospital admissions in California, up nearly 50% from a month earlier.
Covid-19, the flu, and RSV

And it's not just Covid-19. Clinics in Southern California report being busy with other viral illnesses, too – namely flu and respiratory syncytial virus, or RSV.
Notably, Covid-19, flu, and RSV seem to be all "colliding this year," UC San Francisco's Dr. Peter Chin-Hong said. "Last year, RSV would have gone down by now."
Other factors in the spread of Covid-19, which have been seen consistently this time of year since the pandemic began, are holiday travel and gatherings indoors. And in the first holiday season since the end of Covid's emergency phase, people are perhaps not being as cautious as they once were in terms of testing or staying at home if they are sick.
The CDC recommends that virtually everyone age 6 months and older get a fresh Covid-19 and flu vaccination this winter. RSV vaccinations are also available for babies, those age 60 and older, and those who are pregnant.
As of December 9, just 42% of adults nationwide had received a flu shot, 18% had received an updated Covid-19 vaccine, and 17% of those age 60 and up had received an RSV vaccine, according to reports published this week by the CDC. Notably, just one in three nursing home residents were up to date with their Covid-19 vaccinations.
"Many adults who had not received the vaccines reported being open to vaccination," one of the reports said.
How to avoid catching Covid-19

The public health risk posed by JN.1 is similar to other subvariants in the sprawling omicron family, the first version of which emerged a little more than two years ago. While these variants don't pose the same threat as years prior, given a degree of immunity from past infections and immunizations, people who haven't received a recent Covid-19 vaccination – particularly the new formula – are at greater risk.
"JN.1 [and other coronavirus variants] continue to cause disease and too many are falling ill, requiring hospitalizations or advanced clinical care, are dying, and developing long Covid," Maria Van Kerkhove, WHO's technical lead on Covid-19, wrote in a social media post. Nationally, about 1,000 coronavirus-infected people a week are dying.
Health officials have also urged people and healthcare providers to utilize anti-Covid drugs like Paxlovid when possible.
CDC Director Dr. Mandy Cohen and others have urged people to take non-pharmaceutical precautions, such as wearing a mask in public settings, moving gatherings outdoors and improving ventilation, staying home when sick, and avoiding people who are ill.
Other now-familiar measures include using hand sanitizer or regularly washing your hands, especially before eating, after sneezing or coughing, or while in public, the LA County Department of Public Health said.
"Consider talking with friends and family so they know to be cautious about gathering if they show signs of infection," such as having a sore throat or a fever, the agency said. "Event hosts may want to consider asking their guests to test for Covid-19 before celebrations, especially if older or immunocompromised people will be present."
What to do if you test positive for Covid-19
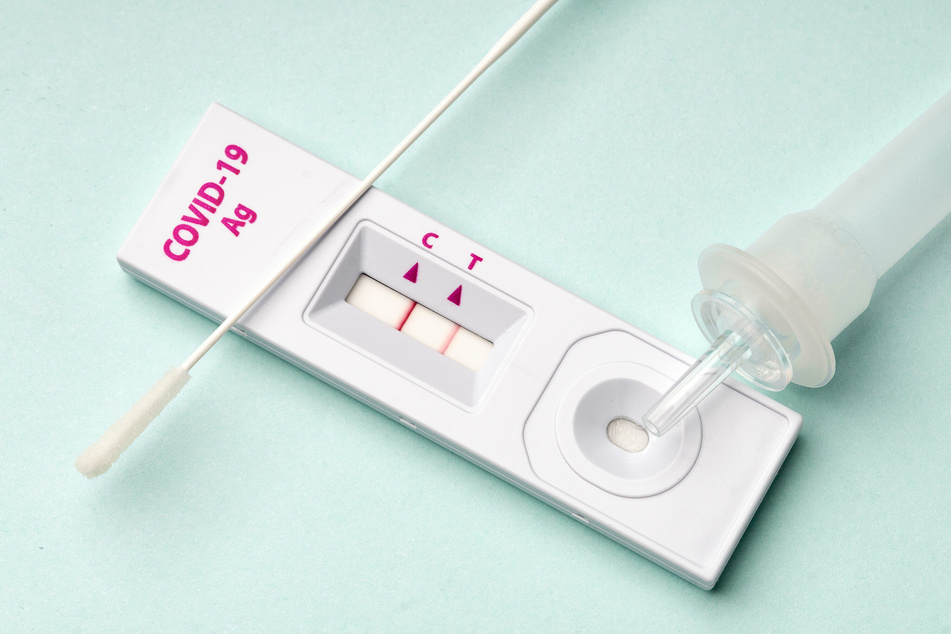
California continues to require most insurers to reimburse covered people for the costs of up to eight at-home Covid tests per month, although people may need to obtain the tests through an "in-network" provider for the tests to remain free.
People who test positive for the coronavirus should isolate for at least five days following onset of symptoms or their first positive test result, whichever came first. The day a person starts having symptoms or had their first positive test is considered Day Zero, and the earliest a patient can exit isolation is by the end of Day 5.
According to the LA County Department of Public Health, infected people can end isolation after Day 5 if they have been fever free for 24 hours without using fever-reducing medications, and don't have any other symptoms, or their symptoms are mild and improving.
The agency strongly recommends people get a negative rapid test result before ending isolation between Days 6 and 10. Isolation can generally end after Day 10 without needing a negative test result, unless you still have a fever.
Infected people are encouraged to wear a mask around others for a full 10 day-period following onset of symptoms or their first positive test. But the agency says that people who meet the criteria to end isolation after Day 5 can stop wearing a mask, too, if they have two consecutive negative coronavirus test results taken at least one day apart.
Cover photo: 123rf/vampy1